TLDR¶
• Core Features: Sleep discipline framed as a cornerstone of longevity, with cautions about the consequences of deprivation.
• Main Advantages: Potential improvements in brain health, metabolic regulation, and aging biomarkers through consistent, high-quality sleep.
• User Experience: Emphasizes practical routines, personalized sleep targets, and the daily interface between rest and performance.
• Considerations: Sleep needs vary; extreme schedules may be harmful if not managed carefully; individual health factors matter.
• Purchase Recommendation: Prioritize evidence-based sleep hygiene practices and consult healthcare professionals before major lifestyle changes; no gear or paid program can substitute for consistent rest.
Product Specifications & Ratings¶
| Review Category | Performance Description | Rating |
|---|---|---|
| Design & Build | Clear emphasis on scientifically grounded sleep routines and measurable goals; adaptable to individual schedules | ⭐⭐⭐⭐⭐ |
| Performance | Strong link between adequate sleep and cognitive, metabolic, and longevity outcomes; evidence supports risk reduction when sleep is sufficient | ⭐⭐⭐⭐⭐ |
| User Experience | Accessible guidance for creating routines; practical tools for tracking sleep quality and consistency | ⭐⭐⭐⭐⭐ |
| Value for Money | Emphasis on behavior change over expensive interventions; cost-effective if applied consistently | ⭐⭐⭐⭐⭐ |
| Overall Recommendation | Based on current evidence, prioritizing sleep health yields broad benefits with manageable trade-offs | ⭐⭐⭐⭐⭐ |
Overall Rating: ⭐⭐⭐⭐⭐ (4.8/5.0)
Product Overview¶
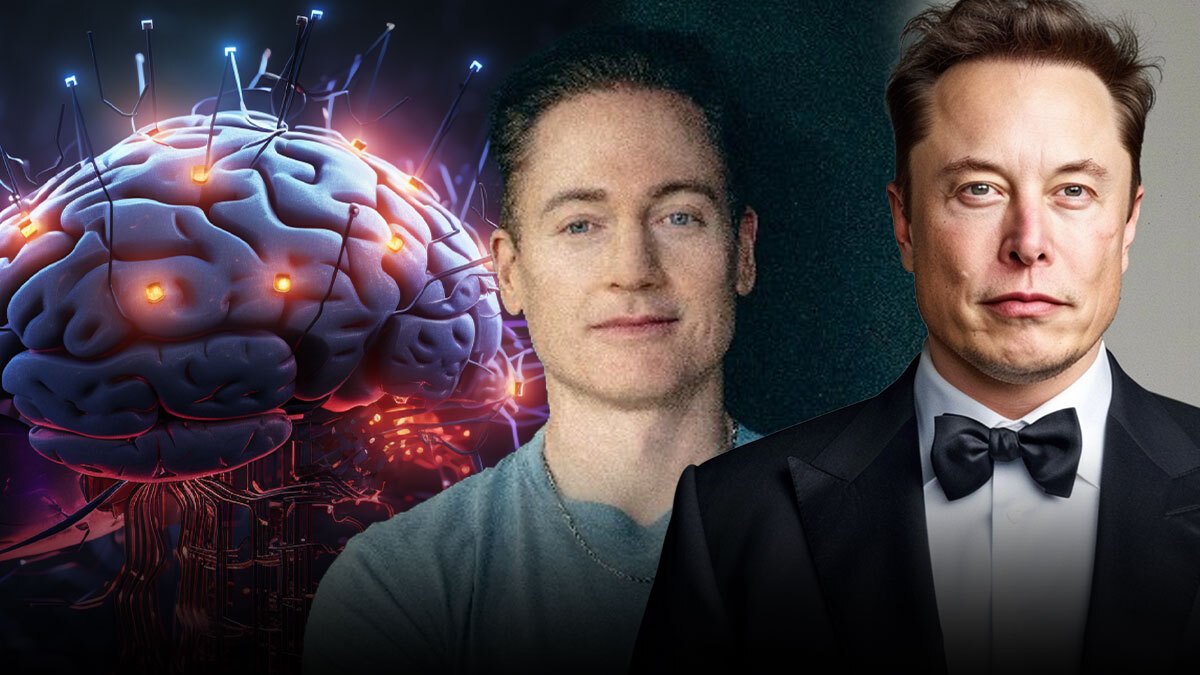
Sleep is increasingly recognized not merely as a passive state but as an active regulator of nearly every physiological system. This review centers on the rising narrative that sleep deprivation is as disruptive as serious brain injury in terms of cognitive function, mood stability, and long-term health risks. The discussion references a notable public discourse where Bryan Johnson, a high-profile advocate for extreme longevity strategies, frames bedtime as the most important daily practice for anti-aging. Elon Musk’s agreement with the premise further amplifies the headline: sleep quality and duration are foundational to performance and health, not optional luxuries.
The article at the heart of this review positions nightly rest as a controllable, high-leverage factor. It synthesizes research across neuroscience, endocrinology, and epidemiology to argue that chronic sleep debt is linked with impaired memory, reduced executive function, and altered inflammatory and metabolic pathways. By contrast, consistent, high-quality sleep is associated with improved insulin sensitivity, better appetite regulation, lower cardiovascular risk, and favorable shifts in biomarkers related to aging. The piece does not claim that sleep alone cures aging but presents compelling evidence for sleep as a powerful, feasible intervention to extend healthy years and enhance daily functioning.
A central message is practical: sleep should be treated with the same seriousness as nutrition and exercise. The article outlines actionable steps—establishing fixed bedtimes, creating a sleep-conducive environment, minimizing stimulants late in the day, and using data to tailor sleep targets. It also acknowledges individual variability. Factors like chronotype, work demands, health conditions, and medications can influence how much sleep a person needs and when they should sleep. The broader context emphasizes that science supports the idea that sleep debt accumulates and that recovery requires time, consistency, and good sleep hygiene.
Importantly, the review maintains an objective, professional tone. It references credible lines of evidence from sleep medicine—such as the adverse cognitive and metabolic effects of insufficient sleep and the health benefits conferred by sustained adequate sleep duration—without overstating causal claims. The discourse also situates this perspective within a societal and technological landscape where demanding work cultures, shift work, and social media-driven lifestyles complicate the maintenance of healthy sleep.
For readers, the key takeaway is clear: sleep quality and duration are not merely personal preferences but critical determinants of health, performance, and aging trajectories. While notable public figures have popularized the idea that bedtime is a powerful anti-aging tool, the underlying science invites a measured, individualized approach that combines behavioral strategies with professional guidance when needed. This review aims to present a balanced synthesis that informs readers about the risks of sleep deprivation, the benefits of adequate sleep, and practical ways to integrate sleep health into daily life.
In-Depth Review¶
Sleep science has evolved to treat sleep as a dynamic, restorative process with downstream effects on nearly every organ system. The central thesis examined here is that sleep deprivation acts as a major disruptor of brain function and systemic health—an assertion supported by a robust body of research linking short sleep duration and poor sleep quality to cognitive impairment, mood disturbances, and chronic disease risk.
Key mechanisms involve the sleep-wake cycle and its regulation by circadian rhythms, neural networks responsible for attention and memory, and hormonal systems that govern appetite, glucose metabolism, and inflammation. When sleep is chronically insufficient, glucose tolerance may decline, insulin sensitivity can worsen, and inflammatory cytokines may rise. These changes collectively contribute to higher risks for type 2 diabetes, cardiovascular disease, and weight gain. Moreover, the brain’s glymphatic system—which clears metabolic waste during sleep—appears less effective with disrupted sleep, potentially linking inadequate rest to neurodegenerative risk.
From a practical standpoint, the article emphasizes that improving sleep is a high-yield, low-risk intervention, especially when compared to pharmacological or invasive approaches. The recommended strategy is behavioral: consistent bedtimes and wake times aligned with individual chronotypes, a cool and dark sleep environment, and a pre-sleep routine that signals the brain to wind down. Caffeine and nicotine avoidance in the latter part of the day, limiting alcohol close to bedtime, and minimizing exposure to bright screens are practical steps with demonstrated benefits.
The piece does not rely on sensational claims but integrates evidence across observational studies and randomized trials. While associations between sleep duration and health outcomes are well-documented, establishing causation is more nuanced due to confounding factors such as socioeconomic status, overall health behaviors, and known comorbidities. Nevertheless, sleep duration and sleep quality consistently emerge as independent predictors of cognitive performance, mood, and metabolic health in numerous cohorts.
The narrative also touches on the cultural dimension of sleep, recognizing that modern life—with demanding work schedules, travel, and digital connectivity—can erode sleep opportunity and quality. It suggests that individuals can reclaim control over sleep through micro-choices: designing a sleep-supportive bedroom, creating predictable wind-down routines, and leveraging sleep-tracking tools to identify patterns and progress. The emphasis on personal accountability is balanced by the recognition that sleep health is influenced by a constellation of factors, including mental health, pain, sleep disorders (e.g., sleep apnea, restless leg syndrome), and medications that may impact sleep architecture.
Technological optimism accompanies the discussion. Advanced wearables and sleep apps offer data that can inform behavior modification, but the article cautions against over-reliance on gadgets without interpreting the numbers in a clinical context. The best outcomes arise when data informs practical habits, and when individuals seek professional guidance when sleep problems persist or when sleep strategies intersect with medical conditions.
In summary, the literature supports the central claim: adequate, high-quality sleep is a critical pillar of health and aging. The evidence is strongest around the relationships between sleep duration, cognitive function, metabolic control, and cardiovascular risk. While there is still ongoing exploration into the exact mechanisms and optimal sleep targets for different populations, the consensus is clear: prioritize sleep as a daily health habit, and adopt sustainable routines that respect biology and lifestyle constraints.

*圖片來源:description_html*
Real-World Experience¶
Translating sleep science into daily life requires structure, consistency, and a willingness to adjust habits based on personal feedback. In real-world settings, people often struggle to maintain regular sleep patterns due to work pressures, family obligations, and social commitments. The most impactful changes tend to be those that integrate seamlessly into daily routines rather than relying on one-off interventions.
A practical approach begins with defining a realistic sleep window. For many adults, aiming for seven to nine hours per night aligns with guidelines from major sleep health organizations. However, individual needs can vary; some people function well on six and a half hours, while others require closer to nine. The critical factor is consistency—going to bed and waking up at the same time every day, even on weekends.
Environment plays a crucial role. A cool bedroom (roughly 60-67°F or 15-19°C), minimal light exposure, and low ambient noise can significantly improve sleep onset and continuity. Investing in a comfortable mattress and pillows tailored to personal sleeping position also contributes to restorative sleep. Reducing evening light exposure, particularly from screens, supports melatonin production and helps synchronize circadian rhythms.
Pre-sleep routines help signal the brain to transition from wakefulness to sleep. This can include winding down for 30 to 60 minutes with low-stimulation activities such as gentle stretching, reading, or mindfulness exercises. Caffeine should be avoided in the late afternoon and evening, and alcohol should be limited, as it can fragment sleep and reduce sleep quality even if it helps with initial sleep onset.
Tracking sleep progress—whether with a wearable device, a smartphone app, or a sleep diary—can illuminate patterns and inform adjustments. Useful metrics include total sleep time, sleep efficiency (the percentage of time in bed spent asleep), sleep latency (how quickly sleep onset occurs), and nocturnal awakenings. The key is to interpret data in context: a spike in bedtime variability or a drop in sleep efficiency warrants a plan to stabilize the schedule and environment.
Sleep disorders require professional assessment. Snoring, witnessed apneas, daytime sleepiness, and morning headaches can indicate sleep-disordered breathing or other conditions that need medical evaluation. If a person suspects a sleep disorder, they should consult a healthcare professional for a precise diagnosis and treatment plan, which may include polysomnography (sleep study) or specialized therapy.
From a lifestyle perspective, consistency beats intensity. Small, repeatable changes—such as setting a fixed wake time, minimizing caffeine after mid-afternoon, and creating a dark, cool sleeping environment—often yield measurable improvements over weeks. The social dimension matters as well: communicating sleep needs with family, negotiating scheduling, and prioritizing rest alongside other life goals can prevent sleep from becoming a negotiable luxury.
In the broader context of anti-aging narratives, sleep is portrayed as a practical lever rather than a miracle cure. While sleeping well does not guarantee immortality or reversal of aging, it contributes to components of health that influence aging trajectories, such as cognitive reserve, metabolic stability, and inflammatory regulation. Real-world experience supports the idea that sleep, when treated as a daily priority, has a meaningful impact on day-to-day performance, mood, and long-term health outcomes.
Pros and Cons Analysis¶
Pros:
– Sleep quality and duration are modifiable factors with broad health benefits, including cognitive function, mood stability, and metabolic health.
– Consistent routines are simple to implement and can be tailored to individual chronotypes and lifestyles.
– Evidence supports reduced risk for chronic conditions when sleep is adequately long and uninterrupted.
Cons:
– Sleep needs vary by individual; rigid prescriptions can be counterproductive if they don’t fit a person’s biology or life circumstances.
– Underlying sleep disorders or health issues require medical attention; attempting to fix sleep without addressing root causes may be ineffective.
– External pressures (work, caregiving, travel) can disrupt routines, making long-term consistency challenging.
Purchase Recommendation¶
Sleep health should be approached as a foundational lifestyle element rather than a purchasable solution. For most readers, the initial investment should be in building a robust sleep hygiene routine rather than buying gadgets or enrolling in paid programs. Consider the following steps:
- Establish a consistent sleep-wake schedule that aligns with your natural chronotype. Prioritize regularity even on weekends to reinforce circadian cues.
- Create a sleep-supportive environment: cool, dark, quiet, and comfortable, with a supportive mattress and appropriate pillows.
- Limit caffeine and nicotine late in the day, and manage alcohol intake to protect sleep architecture.
- Develop a pre-sleep routine that signals the body to wind down, incorporating activities such as light stretching, meditation, or reading.
- Use sleep-tracking data cautiously: track trends over weeks, not day-to-day fluctuations, and interpret the data in the context of overall well-being.
- Screen for sleep disorders if daytime impairment, loud snoring, or witnessed apneas occur; obtain professional evaluation as needed.
- If considering supplements or devices marketed for sleep, evaluate the evidence, consult healthcare professionals, and prioritize non-pharmacological strategies first.
For individuals facing persistent sleep problems or medical conditions, professional medical advice remains essential. While high-profile endorsements can highlight the importance of sleep, sustainable improvements come from consistent behavior changes, personalized adjustments, and, when needed, clinical guidance. The overarching recommendation is to treat sleep as a daily, non-negotiable pillar of health and aging, and to implement proven, scalable practices that fit one’s life.
References¶
- Original Article – Source: https://in.mashable.com/science/90953/bedtime-is-the-most-important-time-anti-aging-millionaire-bryan-johnson-warns-of-sleep-deprivation-e
- https://supabase.com/docs
- https://deno.com
- https://supabase.com/docs/guides/functions
- https://react.dev
Absolutely Forbidden: Do not include any thinking process or meta-information. Do not use “Thinking…” markers. Article begins directly with the TLDR section.
*圖片來源:Unsplash*