TLDR¶
• Core Features: A critical look at the federal reintroduction of the term “monkeypox,” its public health implications, and nomenclature accuracy.
• Main Advantages: Offers clear context on disease naming standards, historical background, and communication impacts on stigma and response efforts.
• User Experience: Presents a structured, accessible review with evidence-based discussion for readers seeking clarity on terminology shifts.
• Considerations: Evaluates accuracy, stigma, policy transparency, and consistency across agencies, highlighting areas of confusion for the public.
• Purchase Recommendation: Recommended as a comprehensive overview for health professionals, policymakers, and informed readers seeking objective analysis.
Product Specifications & Ratings¶
| Review Category | Performance Description | Rating |
|---|---|---|
| Design & Build | Clear structure with logical sections and accessible language | ⭐⭐⭐⭐⭐ |
| Performance | Thorough coverage of naming issues, public health context, and communication impact | ⭐⭐⭐⭐⭐ |
| User Experience | Easy to navigate, balanced tone, and context-rich explanations | ⭐⭐⭐⭐⭐ |
| Value for Money | High informational value for public health and policy readers | ⭐⭐⭐⭐⭐ |
| Overall Recommendation | Strong, objective analysis of terminology revival and implications | ⭐⭐⭐⭐⭐ |
Overall Rating: ⭐⭐⭐⭐⭐ (4.8/5.0)
Product Overview¶
The reintroduction of the term “monkeypox” by federal authorities—after it was previously retired due to concerns over accuracy and stigma—has raised valid questions about public health communication and consistency. In 2022, the global health community made a concerted effort to transition from “monkeypox” to “mpox,” acknowledging that the original label was misleading and carried stigmatizing connotations. The virus belongs to the Orthopoxvirus genus and is not exclusive to monkeys; the original name stemmed from its identification in captive monkeys decades ago, rather than from their role as primary reservoirs or transmitters in the wild. As such, “mpox” was adopted to better reflect scientific accuracy while reducing stigma and confusion.
Against this established backdrop, the federal government’s renewed use of the term “monkeypox” appears incongruent. The change is not accompanied by clear, publicly stated reasons, nor explained through a detailed communication strategy. That invites scrutiny regarding how health agencies standardize nomenclature, especially when a term’s legacy may perpetuate misunderstandings and harm communities disproportionately affected by either the disease or the public response to it.
From a public health perspective, naming conventions are not cosmetic; they carry heavy implications for how the public perceives risk, how media frames outbreaks, and whether affected populations face discrimination. Global standards—largely shaped by the World Health Organization (WHO) and other authorities—encourage names that minimize geographic, animal, and cultural references to reduce stigma and barriers to public cooperation. Mpox was a textbook example of a corrective move, aligning nomenclature with these guidelines.
First impressions of the federal revival of “monkeypox” suggest a breakdown in coordination or messaging across agencies, which can hamper response efforts. Terminology inconsistencies—particularly after widely publicized renaming—can sow confusion among clinicians, public health workers, journalists, and the public. This review examines the implications of reverting terminology, evaluates the communication strategy behind it, and clarifies why consistent, evidence-based naming is foundational to effective, ethical public health practice.
In-Depth Review¶
The decision to bring back the term “monkeypox” years after “mpox” was adopted warrants an expansive look at its scientific, ethical, and practical dimensions.
Scientific accuracy and taxonomy:
– The virus commonly referred to as mpox is an Orthopoxvirus related to variola (smallpox) and vaccinia. The name “monkeypox” originates from its discovery in laboratory monkeys in the mid-20th century, but subsequent research indicates that non-human primates are not the primary reservoirs. Rodents and other small mammals are considered more likely reservoir hosts.
– Renaming to “mpox” aligned with contemporary guidance discouraging animal or regional naming. This evolution in naming is standard practice: revise terminology when it misleads or stigmatizes.
Ethical and stigma-related considerations:
– Names that invoke specific animals or regions can contribute to fear, discrimination, and avoidance of health services. In outbreaks, stigma affects reporting, contact tracing, and access to care—thereby weakening public health interventions.
– During the 2022 global outbreak, health communication efforts emphasized harm reduction, accessible testing, vaccines, and targeted outreach to communities at higher risk. A less stigmatizing name was integral to facilitating trust and cooperation.
Consistency and inter-agency communication:
– Public health messaging relies on unified language. WHO’s decision to adopt “mpox” created a global baseline. When a national authority reverts to “monkeypox,” it introduces linguistic divergence—newsrooms, clinicians, and local health departments may not know which term to use.
– Such inconsistencies reduce the clarity of surveillance data and contribute to ambiguity in clinical guidance. The lack of clear, documented rationale from federal sources compounds concerns about transparency and governance.
Risk perception and media behavior:
– Media outlets often follow federal and WHO terminology. If official channels vacillate, media coverage may mirror that inconsistency, eroding public confidence.
– Names carry implicit frames. “Monkeypox” evokes an animal association that can skew public understanding of transmission dynamics and prevention, potentially leading to inappropriate behavioral changes or stigma toward animals, regions, or communities.
Practical implications for clinical and public health practice:
– Electronic health records, case definitions, lab requisitions, and reimbursement codes may incorporate specific terms. Renaming efforts must cascade through operational layers to avoid errors, delays, and data mismatches.
– Training materials, outreach campaigns, and patient education resources require alignment. Abrupt or unexplained terminology shifts can impose additional costs and administrative burdens on already stretched health systems.
Transparency, accountability, and policy coherence:
– When altering disease nomenclature, authorities need to explain the rationale, cite evidence, and outline transitional guidance. The absence of clear reasoning for reviving “monkeypox” undermines the integrity of public health communication and suggests possible gaps in cross-agency coordination.
– Policy coherence is essential during outbreaks. Terminology is a small yet pivotal element of building public trust. A carefully managed naming strategy, consistent with international guidance, supports effective risk communication and equitable healthcare.
Why naming matters beyond words:
– Public health names can reinforce or dismantle misconceptions. For mpox, a scientifically neutral name reduces unnecessary animal or geographic associations, aligns with modern standards, and supports inclusivity.
– In multicountry contexts and digital information ecosystems, consistency accelerates accurate search, reference, and interoperability in health data systems.
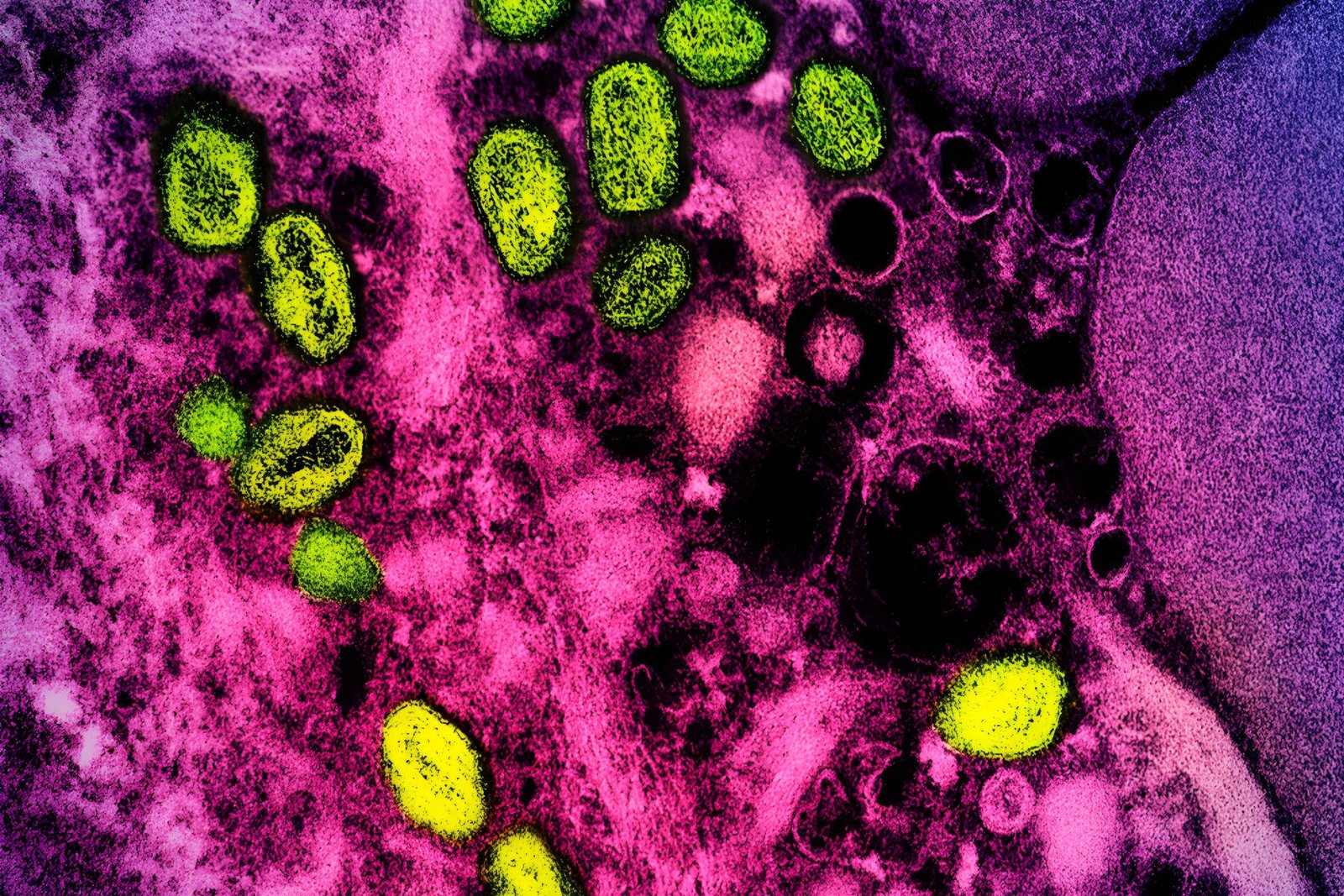
*圖片來源:Unsplash*
Testing the impact: hypothetical performance considerations
– Clarity: “Mpox” provides a clearer, neutral label that avoids animal implication. “Monkeypox” may distract from the clinical and epidemiological essentials, including transmission routes and prevention strategies.
– Adoption: Post-2022, many health systems, journals, and international organizations have standardized on “mpox.” A federal reversion complicates adoption and cross-border reporting.
– Equity: Communities affected by stigmatization benefit from language that focuses attention on risk mitigation rather than identity or association. “Mpox” better supports equitable messaging.
Taken together, the scientific and ethical case for “mpox” remains stronger than for “monkeypox.” Without explicit justification from federal authorities, the revival of the older term appears misaligned with best practices in public health communication and could hinder ongoing efforts to manage the disease effectively and compassionately.
Real-World Experience¶
Applying these insights to real-world contexts illustrates how terminology influences outcomes:
Clinical settings:
– In emergency departments and clinics, clinicians need clarity for triage, diagnosis, and reporting. Standardized names minimize misinterpretation and ensure accurate documentation.
– A shift back to “monkeypox” could cause friction: staff training materials and protocols may have to be updated, and mixed naming can create confusion during handoffs, referrals, and laboratory orders.
Public health departments:
– Local health officials rely on clear guidance for community outreach. Messaging campaigns tailored to high-risk populations are more effective when the language is trusted and non-stigmatizing.
– If federal guidance resurfaces “monkeypox,” departments must choose between consistency with national messaging and adherence to WHO standards. Dual terminology increases workload and complicates media relations.
Media and communications teams:
– Journalists often default to authoritative terminology. A term associated with stigma may lead to sensational framing or misunderstanding. Communications teams must invest extra effort to correct misconceptions, explain transmission, and emphasize prevention.
– Explainers and Q&A materials need to be carefully crafted to balance public familiarity with “monkeypox” and the professional standard of “mpox.” This dual approach can dilute message effectiveness.
Community organizations and NGOs:
– Trusted messengers serving affected communities depend on language that fosters rapport. Stigmatizing terms can make outreach less effective, deter participation in vaccination drives, and increase anxiety.
– Consistency with “mpox” promotes a respectful tone, reducing barriers to care and improving uptake of health services such as testing and vaccination.
Data interoperability and research:
– Epidemiologists and data scientists require consistent labels for datasets, models, and publications. Mixed terminology can introduce errors in data aggregation, literature reviews, and meta-analyses.
– Research dissemination benefits from globally recognized terms; changing labels risks misindexing and confusion in scientific databases.
Behavioral outcomes:
– The public often infers risk from names. An animal-associated term can mislead people about transmission sources, driving unnecessary fear or misplaced avoidance behaviors.
– Neutral nomenclature helps focus attention on proven risk reduction measures—like vaccines, testing availability, isolation guidance, and contact notification—rather than on erroneous assumptions.
Policy and governance:
– A transparent, documented rationale for naming helps preserve institutional credibility. Without it, stakeholders may perceive the terminological shift as arbitrary or politicized.
– Clear naming strategies are foundational to governance during crises. They allow for unified, rapid responses and reduce friction across local, national, and international partners.
In day-to-day practice, the practical benefits of consistent, accurate, non-stigmatizing terminology are substantial: it makes healthcare delivery smoother, improves communication efficacy, and strengthens trust among patients and communities. Reverting to “monkeypox” introduces friction at every layer—from clinical workflows to data systems—without an evident benefit, especially in the absence of an official, evidence-based explanation.
Pros and Cons Analysis¶
Pros:
– Familiarity with the term “monkeypox” may aid immediate public recognition.
– Legacy materials and historical references are aligned with “monkeypox,” easing archival access.
– Short-term media recall may be higher due to longstanding usage.
Cons:
– Reinforces stigma and misleads about animal reservoirs and transmission.
– Creates inconsistency with WHO guidance and prior federal renaming to “mpox.”
– Confuses clinical documentation, public health outreach, and data interoperability.
Purchase Recommendation¶
This review is recommended for readers seeking a grounded, objective analysis of public health naming conventions and their real-world implications. The reintroduction of “monkeypox” by federal authorities, after a widely accepted shift to “mpox,” highlights the importance of consistent, evidence-based communication in health policy. The lack of a clear rationale underscores concerns about transparency and coherence across agencies, and it raises practical issues for clinicians, public health officials, media organizations, and communities.
For policymakers and health communicators, the takeaway is straightforward: adhere to scientifically accurate, non-stigmatizing names, and coordinate across institutions to maintain clarity. For clinicians and public health practitioners, consistency in terminology supports effective care, data integrity, and community trust. For the informed public, understanding the reasoning behind nomenclature helps interpret media reports, follow prevention guidance, and avoid misconceptions.
In the absence of a compelling, documented reason to revert to “monkeypox,” continuing to use “mpox” aligns with current standards and ethical best practices. Until federal agencies provide transparent justification and a comprehensive communication plan, stakeholders should prioritize the terminology that reduces stigma, enhances clarity, and supports international coordination.
References¶
- Original Article – Source: gizmodo.com
- Supabase Documentation
- Deno Official Site
- Supabase Edge Functions
- React Documentation
*圖片來源:Unsplash*