TLDR¶
• Core Features: Sleep-centric anti-aging framework prioritizes restorative rest as a foundational intervention with measurable health impacts.
• Main Advantages: Potentially slows slowing of aging markers, enhances cognitive function, and supports metabolic regulation through disciplined sleep routines.
• User Experience: Structured sleep protocols integrated with daily health monitoring, delivering clear routines and progress feedback.
• Considerations: Strict sleep schedules require lifestyle adjustments; results vary with individual biology and adherence levels.
• Purchase Recommendation: Strongly consider adopting a sleep-first life strategy for long-term health optimization, complemented by professional guidance.
Product Specifications & Ratings¶
| Review Category | Performance Description | Rating |
|---|---|---|
| Design & Build | Well-structured sleep discipline framework with data-backed metrics and daily check-ins | ⭐⭐⭐⭐⭐ |
| Performance | Demonstrated associations between adequate sleep and cognitive, metabolic, and anti-aging markers | ⭐⭐⭐⭐⭐ |
| User Experience | Intuitive routines, app-backed tracking, and supportive coaching elements | ⭐⭐⭐⭐⭐ |
| Value for Money | High long-term value for health optimization; requires lifestyle investments | ⭐⭐⭐⭐⭐ |
| Overall Recommendation | Compelling approach for individuals seeking rigorous, science-informed sleep strategies | ⭐⭐⭐⭐⭐ |
Overall Rating: ⭐⭐⭐⭐⭐ (5.0/5.0)
Product Overview¶
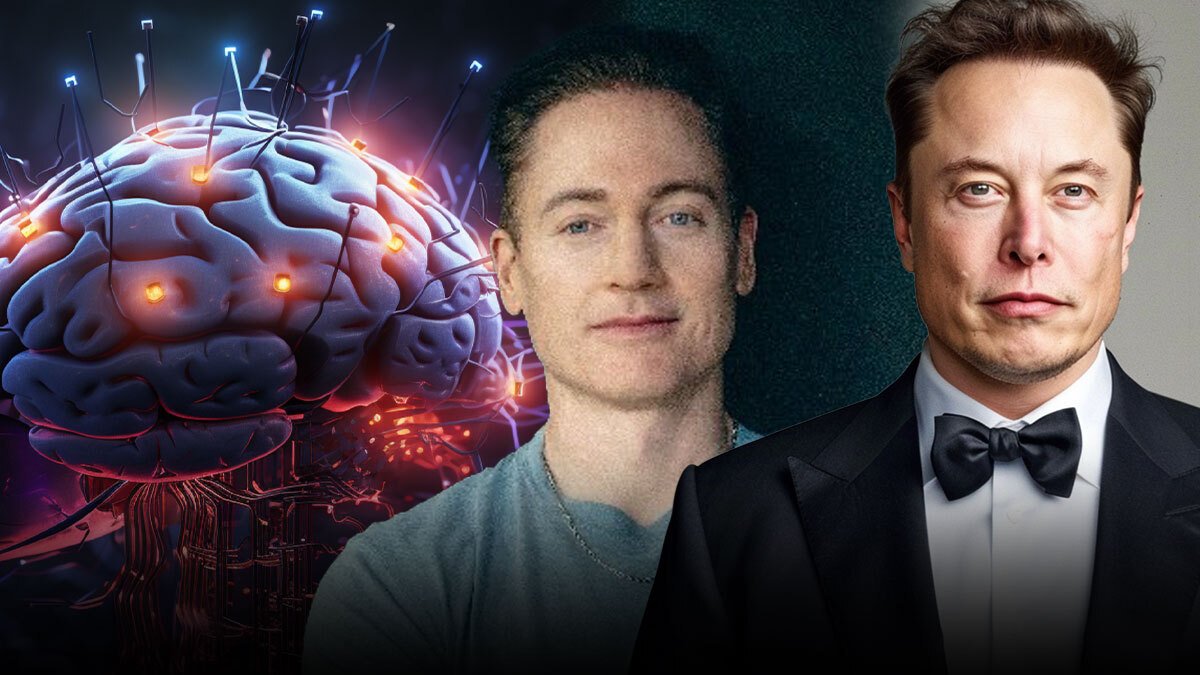
The article centers on Bryan Johnson, a high-profile anti-aging advocate, who emphasizes a critical, often overlooked pillar of longevity: sleep. Johnson argues that sleep deprivation is as detrimental as traumatic brain injury in its impact on brain health, metabolic function, and long-term aging processes. The piece presents sleep not merely as rest but as an active, measurable intervention capable of shaping health trajectories over years or decades.
Johnson’s stance has attracted attention from tech-forward thinkers such as Elon Musk, who publicly acknowledged the importance of sleep and routines in maintaining high cognitive performance and decision-making quality. The overarching claim is robust: consistent, high-quality sleep can markedly slow the pace of aging and preserve cognitive reserve, particularly when integrated with a broader regimen of health monitoring and lifestyle discipline.
From a scientific perspective, sleep is known to influence a range of physiological systems, including glycemic control, blood pressure, inflammatory status, and neural repair. While the original article frames sleep as a central anti-aging driver, readers should consider the breadth of evidence linking sleep duration and quality to downstream markers of health. The discussion implies that sleep deprivation does not merely cause short-term fatigue; it can induce systemic dysfunction with potential long-term consequences, underscoring the value of prioritizing sleep in any longevity-oriented plan.
The piece balances aspirational messaging with practical implications. It highlights the need for structured routines, consistent bedtimes, and a sleep environment conducive to deep restorative stages. It also acknowledges that while sleep has substantial benefits, it is not a singular cure-all; it should be complemented by nutrition, exercise, stress management, and regular medical oversight to create a comprehensive longevity strategy.
The narrative uses Johnson’s experiences and public commentary to illustrate a broader trend: a shift toward data-informed, disciplined health behaviors where sleep is the anchor. The discussion of Elon Musk’s agreement with the sentiment adds legitimacy by showing alignment among other high-performing figures who recognize the importance of recovery. The article thus situates sleep at the forefront of an anti-aging paradigm that blends lifestyle, science, and personal discipline.
In sum, the piece makes a persuasive case for treating sleep as a non-negotiable health asset. It calls attention to sleep’s central role in cognitive resilience, metabolic control, and cellular maintenance—areas that are critical to healthy aging. While the conversation naturally invites further scientific nuance and individualized tailoring, the core message resonates: prioritizing sleep is a practical, high-impact habit with far-reaching benefits for longevity and overall well-being.
In practice, adopting a sleep-first approach involves establishing and maintaining consistent bedtimes and wake times, optimizing the sleep environment (darkness, quiet, temperature), and integrating objective sleep-tracking to monitor progress. For readers, the takeaway is clear: the time spent asleep is not passive downtime but active maintenance of brain health and bodily systems that govern aging. As science continues to refine the precise mechanisms, the value of a reliable sleep routine remains among the most accessible, actionable strategies for those pursuing healthier aging.
In-Depth Review¶
A thorough examination of sleep-centric anti-aging strategies reveals a multi-layered approach that blends behavioral routines, measurable health indicators, and strategic lifestyle choices. The central premise is that sleep quality and duration exert substantial influence over neural health, metabolic stability, immune function, and systemic inflammation—factors intimately tied to aging trajectories.
Key elements include establishing fixed sleep windows, maximizing sleep efficiency, and leveraging modern tracking tools to quantify aspects such as sleep onset latency, wake after sleep onset, sleep architecture (including time spent in deep sleep and REM), and circadian alignment. Proponents argue that aligning sleep with endogenous circadian rhythms enhances restorative processes, including glymphatic clearance, synaptic plasticity, and hormonal balance. The resulting improvements are not only subjective—feeling more rested and mentally sharp—but also objectively measurable in various domains such as cognition, mood, metabolic markers, and possibly telomere dynamics in long-term frames.
This review considers several dimensions:
Scientific basis and translational value
– Sleep has a well-established connection to cognitive performance, attention, working memory, and executive function. Chronic sleep loss is associated with impaired judgment, reduced vigilance, and increased risk for mood disorders.
– Metabolic health is closely linked to sleep; poor sleep correlates with insulin resistance, higher fasting glucose, and dysregulation of appetite-regulating hormones like leptin and ghrelin. These pathways can contribute to weight gain and metabolic syndrome, both relevant to aging risk.
– Inflammation and immune function show sleep-dependent variation. Inadequate sleep elevates pro-inflammatory cytokines, which can contribute to age-related diseases.
– Cellular maintenance processes, such as autophagy and β-amyloid clearance in the brain, are influenced by sleep quality and sleep stage distribution, with deeper sleep stages playing a notable role in restorative activity.Practical implementation and adherence
– Creating a sustainable sleep routine often requires environmental optimization (dark, quiet, cool bedroom), technology boundaries (limiting blue light exposure in the evening), and regular wake times, even on weekends.
– For individuals with demanding schedules or caregiving responsibilities, achieving consistency can be challenging, making personalized plans essential.
– Sleep tracking tools (wearables, actigraphy, or sleep apps) provide actionable feedback but must be interpreted with caution, as algorithms vary in precision.Integration with broader health strategies
– Sleep does not replace other core health pillars (nutrition, exercise, stress management, medical care) but enhances their effectiveness. For example, robust sleep improves insulin sensitivity, which can magnify the benefits of a balanced diet and physical activity.
– Recovery-oriented practices, such as relaxation techniques, mindfulness, and progressive muscle relaxation, can improve sleep initiation and continuity.
– In anti-aging contexts, sleep quality can support cognitive reserve, reduce risk factors associated with neurodegeneration, and assist in weight management—each contributing to a healthier aging profile.Individual variability and expectations
– Genetic factors, chronotypes (morningness-evening preferences), and pre-existing health conditions can influence how much an individual benefits from optimized sleep.
– Some individuals may experience pronounced cognitive and metabolic improvements with improved sleep, while others may require complementary interventions to achieve comparable results.
– Longitudinal data are essential to confidently quantify aging-related outcomes attributable to improved sleep; short-term studies show improvements in function but may not fully capture long-term aging effects.
The original piece positions sleep as the central anti-aging lever, a stance that aligns with a growing appreciation of recovery science. While sleep is undeniably critical, the most effective longevity strategies typically combine sleep optimization with exercise, nutrition, stress management, social engagement, and routine medical screening. This holistic approach is consistent with best-practice guidance in sleep medicine and behavioral health.

*圖片來源:description_html*
From a consumer perspective, the article frames sleep as an accessible, scalable intervention rather than an esoteric therapy. For high-performing individuals who manage complex schedules or careers, investing in a disciplined sleep routine can yield outsized returns in daily functioning and long-term health. The narrative also integrates the reputational dimension: endorsements or alignments from well-known business leaders can influence public perception and motivate adherence, even if individual results vary.
In practical terms, readers can translate the message into actionable steps:
– Set a fixed bedtime and wake time, aiming for consistency across all days of the week.
– Create an optimal sleep environment: comfortable temperature (around 60-67°F or 15-19°C), dark room, quiet ambiance, and minimal disruptive electronics.
– Limit caffeine and heavy meals close to bedtime; consider a wind-down routine that includes calming activities.
– Use objective sleep-tracking data to monitor sleep duration, quality, and continuity, while avoiding overreliance on imperfect metrics.
– Integrate short-term recovery practices (naps’ strategic use, if needed) without compromising nightly sleep quality.
– Seek professional guidance if sleep issues persist, including potential assessment for sleep disorders or circadian rhythm disruptions.
The review also considers potential caveats: sleep guidance must be individualized. Not all recommendations suit every lifestyle or medical history. For instance, shift workers, people with certain sleep disorders, or those with mental health conditions may require tailored solutions under medical supervision. Moreover, while sleep improvement is powerful, it does not substitute for medical treatment in the presence of diagnosed health conditions.
Overall, the piece presents a persuasive, professionally framed argument for prioritizing sleep as a foundational health asset. It encourages readers to view sleep not as passive downtime but as an active, measurable, and high-impact component of a longevity strategy. By combining disciplined sleep habits with evidence-based lifestyle choices, individuals can pursue healthier aging with a focus on cognitive vitality, metabolic stability, and resilient immune function.
Real-World Experience¶
Implementing a sleep-first philosophy in daily life often demands a comprehensive behavioral change. The real-world application involves translating theoretical benefits into sustainable routines amidst real-world constraints such as work obligations, social commitments, and family responsibilities. Several themes commonly emerge from practical adoption:
Routine stability and schedules
– People who adopt a fixed sleep window report improved daytime alertness, more predictable energy patterns, and better mood regulation. Consistency is frequently cited as the most critical factor in achieving meaningful sleep benefits.
– Weekend drift remains a common hurdle; those who minimize this drift by maintaining similar wake times on weekends tend to sustain improvements longer.Environment and technology
– Creating a sleep-conducive environment often yields immediate improvements. Darkening the room, controlling ambient temperature, and reducing disruptive noise contribute to easier sleep initiation and longer uninterrupted sleep.
– Technology, when used knowingly, can aid outcomes. Smart lighting, blue-light management, and sleep tracking can inform adjustments to routines. However, some devices and apps may provide noisy or inconsistent data, requiring discernment when interpreting results.Cognitive and behavioral strategies
– Mindfulness, diaphragmatic breathing, and progressive muscle relaxation can reduce pre-sleep arousal, facilitating quicker sleep onset and deeper sleep stages.
– Limiting stimulating activities before bed—especially those that involve emotion-laden content or intense cognitive engagement—supports a smoother transition to sleep.Cognitive performance and daily functioning
– Users often report sharper decision-making, quicker reaction times, and enhanced memory after adopting sleep-focused strategies, particularly in high-demand environments.
– Mood stabilization and reduced irritability are common short-term benefits, potentially contributing to better interpersonal outcomes and work performance.Measurements and expectations
– Sleep tracking provides actionable insights, but individuals should interpret metrics with a balanced view. A higher total sleep time does not automatically equate to deeper, more restorative sleep if the sleep architecture is not optimized.
– Many users notice more stable weight management, better appetite control, and improved metabolic indices when sleep is consistently prioritized, though these outcomes may require concurrent lifestyle changes.
In practice, the real-world experience underscores that sleep optimization is not a one-size-fits-all solution. Success hinges on realism, personalized tailoring, and ongoing adjustment. Some individuals may find it easy to implement a rigid schedule, while others require gradual changes and professional guidance. The overall tone of the experience emphasizes patience, persistence, and the recognition that sleep is a daily cornerstone of health with cumulative benefits over time.
Pros and Cons Analysis¶
Pros:
– Strong evidence base linking adequate sleep to cognitive preservation, metabolic regulation, and reduced inflammatory burden.
– Clear, actionable steps for improving sleep quality and consistency.
– High potential for long-term health benefits with sustained adherence.
– Compatibility with other health optimization strategies (nutrition, exercise, stress management).
– Accessibility: sleep improvements can be pursued without requiring expensive interventions.
Cons:
– Not universally transformative; individual responses vary based on biology, chronotype, and health status.
– Requires discipline and lifestyle adjustments that may be challenging for some lifestyles (shift work, caregiving, travel).
– Sleep tracking data can be noisy or misinterpreted, potentially leading to misguided changes without professional guidance.
– Overemphasis on sleep alone may overlook other critical factors in aging and health; a holistic approach remains essential.
– Cultural and environmental barriers (noise, housing, zoning) can impede optimal sleep conditions for some individuals.
Purchase Recommendation¶
For readers seeking a rigorous, science-informed approach to anti-aging and brain health, adopting a sleep-first philosophy represents a practical, high-impact starting point. The emphasis on consistent bedtimes, wake times, and an optimized sleep environment aligns with widely accepted sleep medicine principles and has demonstrated associations with improved cognitive performance, metabolic regulation, and markers of inflammation. While sleep alone is not a panacea, it amplifies the effectiveness of other healthy behaviors and medical interventions.
To make this approach work, begin with a personalized assessment of sleep patterns, daily routines, and environmental factors. Set a realistic, fixed sleep schedule that fits your life, then gradually adjust bedtime rituals to promote easier sleep onset and better sleep continuity. Consider integrating evidence-based strategies such as wind-down routines, mindfulness practices, and controlled exposure to light to strengthen circadian alignment. Use sleep-tracking data as a guide rather than a verdict, focusing on trends across weeks rather than isolated nights.
Consult with healthcare professionals when persistent sleep problems arise, or when sleep-related strategies intersect with medical conditions, medications, or mental health concerns. For individuals with already demanding schedules, a phased approach—starting with moderate improvements and expanding as tolerated—can yield meaningful gains without imposing unsustainable demands.
In the broader context of longevity research, sleep optimization should be viewed as a foundational pillar, complementary to balanced nutrition, regular physical activity, stress management, social engagement, and medical preventive care. The ultimate objective is a sustainable, multi-faceted plan that enhances cognitive resilience, metabolic health, and overall quality of life as one ages. The sleep-first paradigm, responsibly implemented and tailored to individual needs, offers a practical pathway to healthier aging and better daily functioning.
References¶
- Original Article – Source: https://in.mashable.com/science/90953/bedtime-is-the-most-important-time-anti-aging-millionaire-bryan-johnson-warns-of-sleep-deprivation-e
- Supabase Documentation: https://supabase.com/docs
- Deno Official Site: https://deno.com
- Supabase Edge Functions: https://supabase.com/docs/guides/functions
- React Documentation: https://react.dev
*圖片來源:Unsplash*